Urgent Care Billing Services
Fast, Accurate, AI-Powered Billing for High-Volume Urgent Care Centers
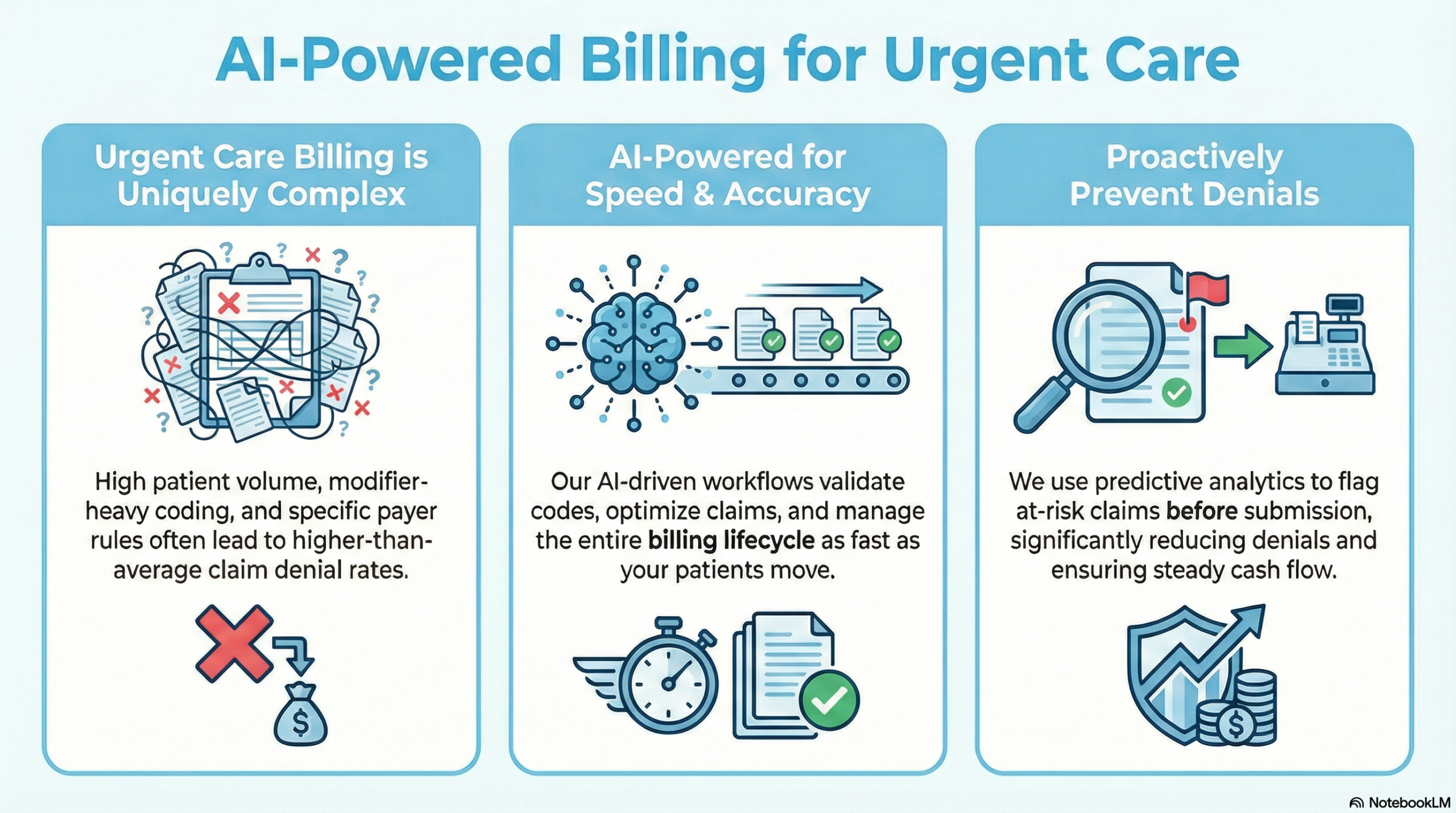
Urgent care centers operate at a rapid pace; high patient volume, walk-in visits, extended hours, and a wide mix of services. That speed creates unique billing challenges that generic medical billing companies often fail to handle properly.
At BillVolt, we deliver specialized urgent care medical billing and revenue cycle management (RCM) built to keep cash flow steady, denials low, and compliance airtight.
Our AI-driven workflows are designed for urgency; so your claims move as fast as your patients.


Why Urgent Care Billing Is Uniquely Complex
Urgent care billing sits between primary care and emergency medicine, which creates challenges such as:
High-frequency E/M services (99202–99215) with variable acuity
Time-sensitive claim submission requirements
Frequent use of procedure codes, diagnostics, X-rays, and injections
Modifier-heavy billing (–25, –59, –91, etc.)
Payer confusion around place of service (POS 20 vs POS 11)
Higher denial rates due to medical necessity and documentation gaps
BillVolt understands these nuances and optimizes every claim for speed, accuracy, and payer acceptance.
Our Urgent Care Billing & RCM Services
BillVolt delivers specialized urgent care billing and revenue cycle management built for high-volume, fast-paced environments. From accurate coding and modifier optimization to denial prevention and A/R follow-up, our AI-powered workflows help urgent care centers get paid faster with fewer rejections and less administrative strain.
End-to-End Urgent Care Revenue Cycle Management
We manage the full billing lifecycle so your staff can stay focused on patient care:
- Real-time eligibility verification
- Accurate charge capture
- ICD-10 and CPT coding validation
- Modifier optimization
- Claim scrubbing and submission
- Denial management and appeals
- Payment posting and A/R follow-up
AI-Assisted E/M & Procedure Coding
Our AI-assisted coding review ensures proper E/M leveling and correct pairing of procedures with diagnoses; reducing undercoding, overcoding, and payer rejections.
Diagnostic & Ancillary Service Billing
We specialize in urgent care billing for:
- X-rays and imaging
- Rapid tests and lab services
- Injections and infusions
- Minor procedures and wound care
Each service is coded and documented to meet payer-specific rules.
Denial Prevention for High-Volume Claims
BillVolt uses predictive denial analytics to flag risk patterns before claims are submitted—significantly reducing:
- Duplicate claim denials
- Medical necessity rejections
- Modifier-related denials
- POS and provider enrollment errors
Common Urgent Care Billing Challenges We Solve
Our approach focuses on clean claims, fast turnaround, and predictable reimbursement.
- Lost revenue from missed modifiers
- Delays caused by POS mismatches
- High denial rates from commercial payers
- Inconsistent documentation across providers
- Growing A/R due to claim volume
Why Urgent Care Centers Choose BillVolt
- Urgent care specific billing expertise
- AI-powered claim validation and denial prevention
- HIPAA-compliant and secure systems
- Transparent reporting and performance dashboards
- Scalable support for single locations or multi-site groups
We adapt to your volume; not the other way around.
Optimize Your Urgent Care Revenue Without Slowing Down
If your urgent care center is struggling with denials, delayed payments, or billing bottlenecks, BillVolt can help. See how AI-powered RCM keeps your revenue moving as fast as your practice.

Frequently asked questions (FAQs)
FAQs About Urgent Care Billing Service
What CPT codes are common in urgent care billing?
Urgent care commonly uses E/M codes (99202–99215), procedure codes, diagnostic tests, imaging, and injection-related CPT codes.
How does BillVolt handle POS 20 vs POS 11 issues?
We validate place-of-service coding at the claim level to ensure alignment with payer rules, preventing unnecessary denials.
Can BillVolt reduce urgent care denial rates?
Yes. Our AI-driven claim scrubbing and modifier validation significantly reduce common urgent care denials.
Is BillVolt compliant with payer and HIPAA regulations?
Absolutely. All workflows are HIPAA-compliant and aligned with CMS and commercial payer billing guidelines.
