The healthcare industry is entering a defining era of transformation; and for those who have been paying attention, this moment didn’t arrive overnight. Years ago, the previous owner of the company I worked for predicted a future where Revenue Cycle Management would no longer be able to keep up by reacting to problems after they occurred. He foresaw rising operational costs, relentless payer scrutiny, workforce shortages, and patients demanding a clearer, more transparent financial experience; factors that would force a fundamental change in how revenue is managed.
Back then, he encouraged us to work tirelessly; days, nights, and even weekends; to automate and innovate, long before these challenges became urgent. His vision allowed us to stay ahead of the curve.
Today, as we move into 2026 and beyond, we have now fully realized the truth of that prediction. Healthcare organizations are being forced to rethink how revenue is captured, protected, and optimized. The future of RCM is no longer reactive; it is predictive, automated, and deeply patient centered, designed to anticipate issues before revenue is lost.
Understanding what’s coming next is no longer optional. It’s essential for financial survival in an industry rapidly redefining how care is delivered and paid for.
Why the Future of RCM Demands Immediate Attention
Healthcare organizations are operating with tighter margins while administrative complexity continues to grow. Payers are enforcing stricter rules, documentation requirements are expanding, and reimbursement timelines are becoming less predictable.
At the same time, patients now expect transparency, convenience, and clarity when it comes to their financial responsibility. The organizations that adapt early will be positioned to thrive, while those that delay will struggle with rising denials, revenue leakage, and operational inefficiencies.
Major RCM Trends Shaping 2026 and Beyond
- Automation and Artificial Intelligence Will Redefine RCM Operations
By 2026, intelligent automation will be embedded into many stages of the revenue cycle, if not all. Tasks that once required hours of manual work; such as eligibility checks, claim validation, and payment posting; will be handled in seconds.
Artificial intelligence and rules-based systems will continuously analyze payer behavior, identify billing risks, and optimize workflows in real time. Instead of chasing problems after they occur, organizations will prevent them before they impact revenue.

- Denial Management Will Become Predictive Rather Than Reactive
Denials will remain one of the most significant threats to healthcare revenue, but how organizations handle them will fundamentally change. Advanced analytics will identify patterns that lead to denials before claims are ever submitted.
This shift will dramatically reduce rework, shorten reimbursement timelines, and improve overall financial performance. Teams will focus less on fixing errors and more on preventing them.
- Value-Based Care Will Reshape Revenue Strategy
As reimbursement models continue to evolve, revenue will be increasingly tied to outcomes rather than volume. This shift requires deeper alignment between clinical documentation, quality reporting, and financial workflows.
RCM teams will need greater insight into performance metrics, risk adjustment, and long term population health outcomes. Financial success will depend on accuracy, collaboration, and data driven decision-making.
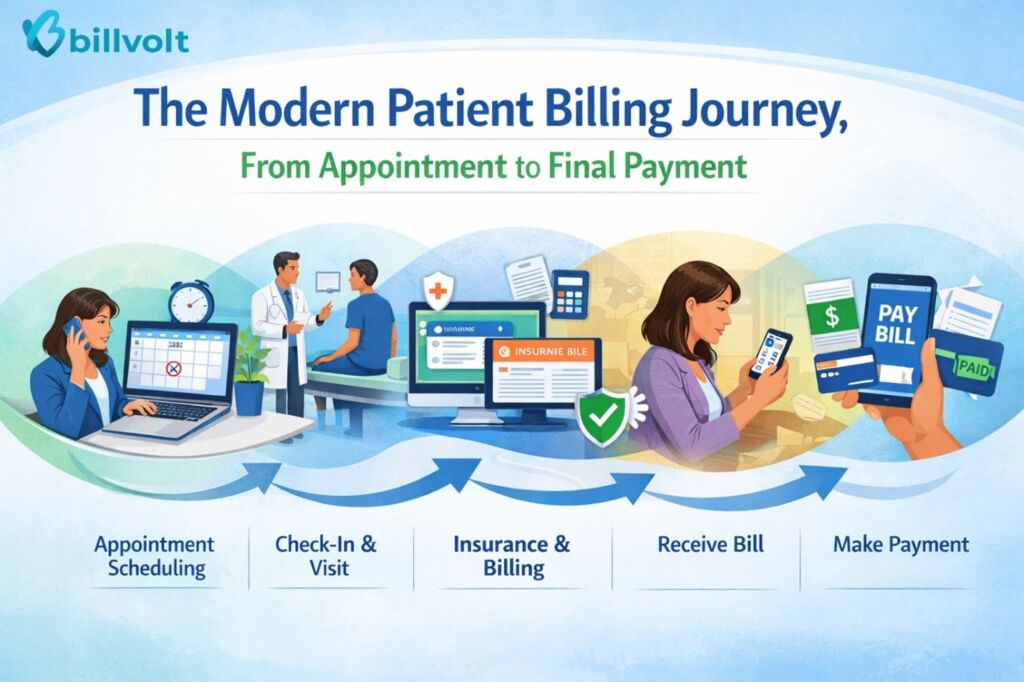
- Patient Financial Experience Will Directly Impact Cash Flow
Patients are no longer passive participants in healthcare billing. They expect clear estimates, digital payment options, and transparent communication.
In the future, successful RCM strategies will prioritize the patient journey from scheduling through final payment. Simplified statements, real-time cost visibility, and flexible payment options will significantly improve collections while strengthening patient trust.
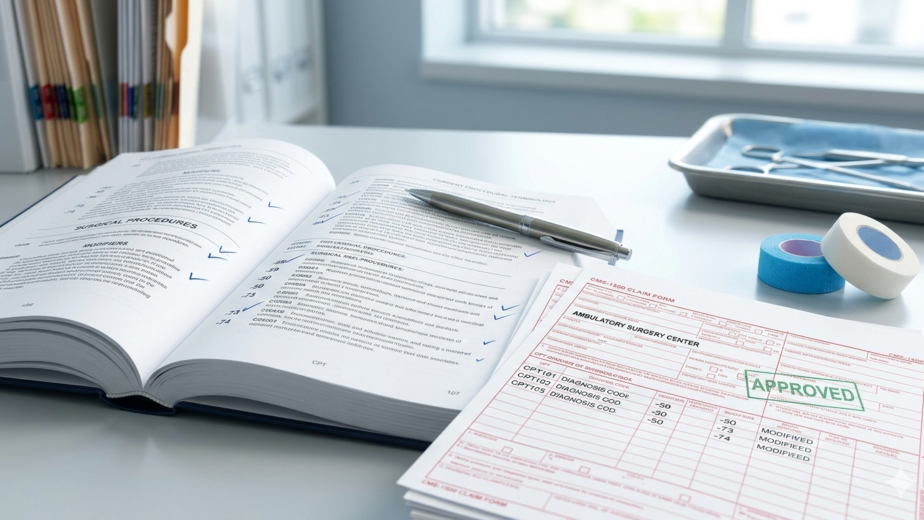
- Regulatory Pressure and Compliance Requirements Will Intensify
Healthcare regulations will continue to grow in complexity. Frequent coding updates, payer policy changes, and increased audit activity will require constant vigilance.
Organizations that fail to keep up will face delayed payments, penalties, and compliance risks. The future of RCM will demand continuous education, strong internal controls, and advanced monitoring tools.
- Outsourced RCM Partnerships Will Become the Norm
Staffing challenges and rising operational costs are accelerating the shift toward outsourced and hybrid RCM models. By 2026, many practices will rely on specialized billing partners equipped with advanced technology and regulatory expertise.
Outsourcing will allow healthcare organizations to scale efficiently, reduce overhead, and maintain consistent revenue performance without expanding internal teams.
Stop Fixing Denials - Start Preventing Them.
The era of reactive billing is over. If your team is still chasing unpaid claims after they’ve been rejected, you’re already behind the curve. See how BillVolt uses predictive insights to stop revenue leakage before it happens.
Challenges Medical Practices Must Prepare for Now
Despite technological progress, challenges remain unavoidable:
- Increasing payer denials
- Workforce shortages and burnout
- Technology adoption barriers
- Data integration complexities
- Growing patient financial responsibility
Proactive planning today will determine financial stability tomorrow.
How Practices Can Prepare for the Future of RCM
- Invest early in intelligent automation and analytics
- Strengthen front-end financial workflows
- Improve collaboration between clinical and billing teams
- Focus on patient-friendly billing processes
- Partner with forward thinking revenue cycle experts
Preparation isn’t about reacting to change, it’s about leading it.
The Road Ahead for Revenue Cycle Management
By 2026 and beyond, Revenue Cycle Management will be proactive, data-driven, and patient-focused; and organizations that fail to evolve risk lost revenue and operational strain. Providers that modernize their RCM strategies now will gain a competitive advantage by improving cash flow, reducing inefficiencies, and delivering a better patient financial experience.
BillVolt is built to help healthcare organizations overcome these challenges and win in the next era of RCM. With advanced technology, proven expertise, and dependable financial performance, BillVolt empowers providers to accelerate reimbursement, strengthen revenue integrity, and scale with confidence. Connect with BillVolt today to transform your revenue cycle for 2026 and beyond, so your organization can grow stronger while staying focused on exceptional patient care.
Will Your Revenue Strategy Survive 2026?
The transition to value-based care and automated RCM isn’t a future possibility—it’s a current requirement for survival. Partner with a forward-thinking revenue cycle expert that scales your practice through intelligent innovation.Contact us today and we will love to chat!